Living with Celiac Disease: What They Don't Tell You at Diagnosis
By Maria Anwar
When I was diagnosed with celiac disease, I thought avoiding bread and pasta would be enough. I quickly learned that living truly gluten-free is far more complex, and I'm sharing my experience to help newly diagnosed individuals understand what lies ahead.
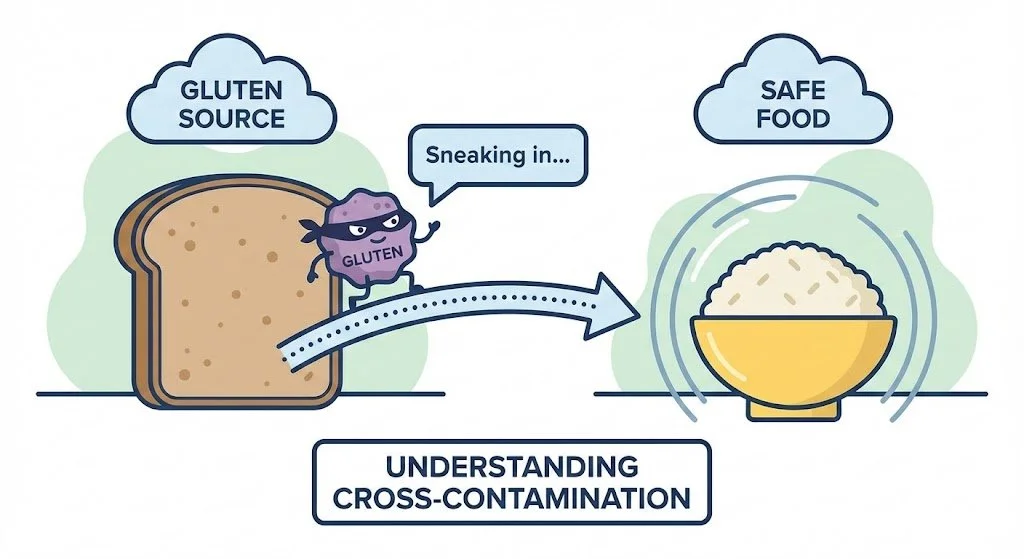
The Tiny but Mighty Truth Behind Gluten-Free Limits
The FDA permits the "gluten-free" label on foods containing less than 20 ppm (parts per million) of gluten. But what is 20 ppm? It means that for every million parts of the food, less than 20 parts can be gluten. To visualize this: imagine a 500g jar of food—at 20 ppm, it could contain around 10 mg of gluten, which is roughly the weight of a few grains of salt. It's incredibly small—but in the battle against gluten, even the tiniest enemy can cause big trouble. Think of yourself as a superhero fighting an army of molecular minions!
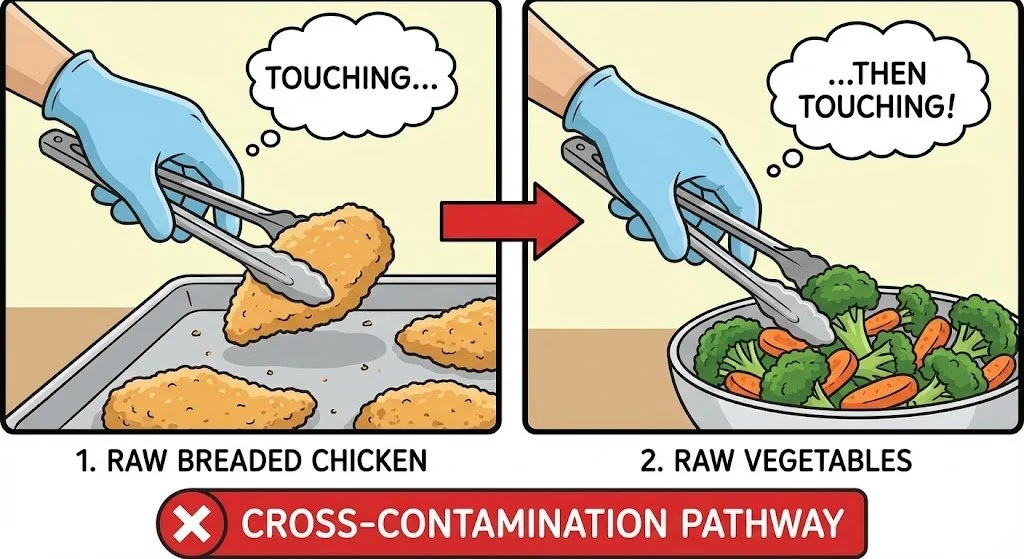
Cross-Contamination: The Hidden Enemy
Cross-contamination is more serious than most realize. A butter knife touched to toast contaminates the entire butter container. A spatula on a counter where bread crumbs once sat can pick up enough gluten to make you sick. Shared cutting boards, toasters, colanders, wooden spoons, flour in air vents—all became threats I had to eliminate.
I needed separate cooking utensils, prep surfaces, and condiment containers. A single crumb on the counter could contaminate my meal. This wasn't paranoia; it was protecting my intestines from damage. I treat a stray breadcrumb with the same level of chill as a live grenade.
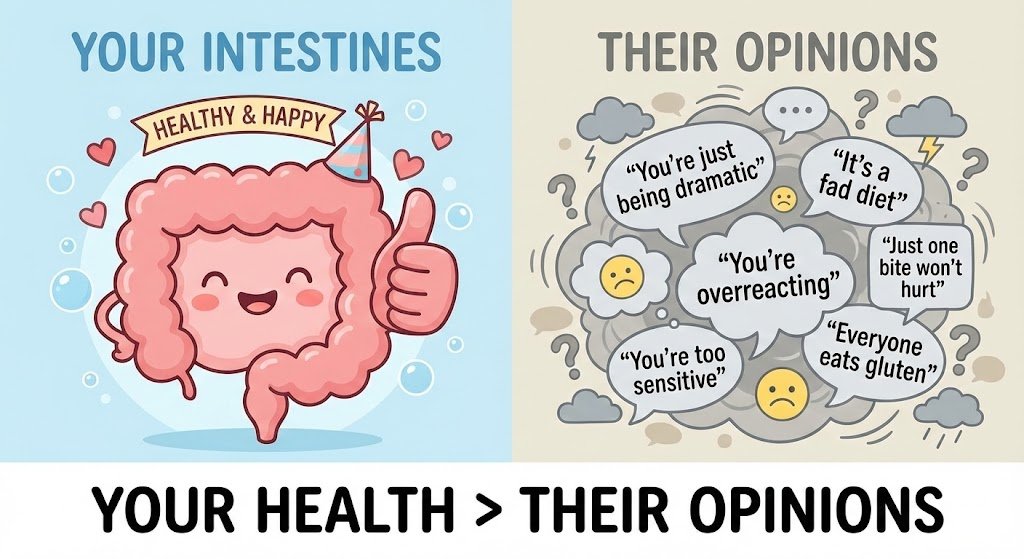
Learning to Say No—And Standing Firm
This is perhaps the hardest part. Because Celiac disease affects ~1% of the population, even friends and family may not understand. Some will accuse you of being overly cautious, diagnose you with OCD, or claim you're following a "fad diet" to look cool. Let’s be honest, nobody pays $8 for a loaf of bread the size of a sponge just for the 'fashion. Unlike diseases like diabetes, which people recognize, celiac disease is rare enough that people feel entitled to mock it.
Do not listen to them. This is not a choice or a trend—it's an autoimmune disease. When someone offers you food that isn't safe, a simple "No, thank you, I have Celiac disease" is enough. You don't owe anyone detailed explanations. Your intestinal health matters more than their comfort. Real friends will respect your boundaries.
The Healing Journey: Patience Required
Once you start a gluten-free diet, your gut needs substantial time to heal. Even when perfectly careful, I had symptoms for weeks. Celiac causes intestinal damage, and those villi (small hairlike structures that absorb food) need time to regenerate. Continued symptoms during healing don't mean you're failing or eating gluten. Your body is recovering. Basically, your intestines are doing a system reboot, but unfortunately, they are running on 1990s dial-up internet.
Moving Forward
With time, vigilance becomes habit. Your energy returns, digestion heals, and you learn to navigate this reality. The key is understanding that "gluten-free" means truly gluten-free— no exceptions. Your health depends on it, and you deserve to feel well again. Just remember you’re not restricted; you’re just exclusive. Very, very exclusive.